Définition
Le syndrome de fatigue chronique est une maladie acquise affectant tous les systèmes corporels, principalement (surtout) les systèmes neurologique, endocrinien et immunitaire. Cette maladie est très mal comprise par les patients, les professionnels de la santé et les chercheurs (1).
Les signes et les symptômes (1)
- une apparition soudaine de fatigue grave, durable et qui diminue grandement les activités du patient; elle peut se combiner à une exténuation, à de l’épuisement, à de la faiblesse, à une sensation de lourdeur et à plus d’efforts au mouvement;
- un sentiment de grande fatigue qui persiste plus de 24 heures après un très petit travail physique ou mental;
- un sommeil non réparateur (sommeil, après lequel les personnes ne se sentent pas reposées);
- une douleur musculaire qui se déplace, parfois sans raison évidente; une douleur à une articulation sans rougeur ni œdème;
- un mal de tête;
- une diminution de la mémoire ou de la concentration;
- un mal de gorge récurrent;
- les ganglions sympathiques fragiles : le plus souvent sur les côtés du cou et sous les bras;
- un étourdissement ou une faiblesse en position debout;
- une sensibilité à la lumière, au bruit et aux odeurs;
- une nouvelle sensibilité aux aliments/aux médicaments/aux produits chimiques;
- des problèmes gastro-intestinaux comme le syndrome du côlon irritable.
Les causes (2)
La flore intestinale
De nombreuses études ont démontré qu’un déséquilibre de l’écosystème intestinal est responsable de ce syndrome de fatigue chronique.
La prédominance d’une flore “amie” du tube digestif permet d’éviter la production de particules inflammatoires, responsables d’une augmentation du stress oxydant et de l’inflammation.
La fonction de barrière intestinale
Pour se protéger des réactions inflammatoires non contrôlées, l’épithélium intestinal a développé des mécanismes pour limiter la croissance bactérienne en limitant le contact direct avec les bactéries, et en empêchant la dissémination bactérienne dans les tissus sous-jacents. Cette barrière intestinale se composant d’une seule couche de cellules épithéliales est un élément important du système immunitaire inné. Elle sépare l’intérieur du corps d’un environnement extérieur très «sale». Ainsi, la fonction de la barrière muqueuse est un élément clé dans l’arsenal des mécanismes de défense nécessaires pour prévenir l’infection et l’inflammation.
La fonction de barrière de la muqueuse est assurée par la sécrétion de mucus, de chlorure ainsi que par la sécrétion d’eau mais également par le fait que ces cellules sont étroitement liées les unes aux autres par un système de jonctions serrées au niveau de leur pôle apical. Ces différents mécanismes contribuent à assurer l’intégrité physique et fonctionnelle de cette barrière intestinale.
Un dysfonctionnement de cette barrière muqueuse se produit dans le syndrome de fatigue chronique. Le stress psychologique perturbe également la barrière intestinale permettant l’entrée des antigènes et des micro-organismes engendrant une réponse excessive du système immunitaire se situant sous la muqueuse intestinale.7
Une perméabilité anormale de cette barrière causée par une destruction des jonctions serrées induit une inflammation, cette nouvelle approche du syndrome de fatigue chronique offre de nouvelles options thérapeutiques ciblant la correction de cette hyperperméabilité par une diététique appropriée et la prescription de compléments nutritionnels (28).
Par conséquent, tout dysfonctionnement de la barrière muqueuse provoque une altération de la motilité intestinale, des sécrétion intestinales et des douleurs abdominales cadrant avec l’un des symptômes rencontré dans le syndrome de fatigue chronique : le syndrome de l’intestin irritable.
Le stress oxydant
De nombreuses publications ont démontré que le syndrome de fatigue chronique est associé à un excès de stress oxydant.
Le stress oxydatif survient lorsqu’il existe un net déséquilibre entre la production de radicaux libres (molécules très réactives, liées à l’oxygène) qui si ils ne sont pas neutralisées par des antioxydants détruisent nos tissus.
Le sulfure d’hydrogène
L’altération de la flore intestinale peut avoir des conséquences graves pour la santé de l’hôte. Les bactéries pathogènes en surpopulation dans la cavité buccale et le tractus gastro-intestinal produisent au contact de métaux lourds le sulfure d’hydrogène “gaz toxique” ayant une odeur caractéristique d’œufs pourris (H2S). Le sulfure d’hydrogène est un inhibiteur de la respiration mitochondriale, plus puissant que le cyanure, bloquant la production d’énergie (ATP) par la mitochondrie, ce qui explique cette fatigue chronique.
Le sulfure d’hydrogène est un inhibiteur de la respiration mitochondriale, plus puissant que le cyanure, bloquant la production d’énergie (ATP) par la mitochondrie, ce qui explique cette fatigue chronique.
Cette surproduction d’H2s est également responsable de la destruction de la barrière intestinale entretenant le cercle vicieux de l’inflammation.
Dysfonctionnement mitochondrial
La mitochondrie est l’organite intracellulaire qui produit notre source universelle d’énergie : l’ATP (adénosine triphosphate). lorsque nos mitochondries fonctionnent correctement nous produisons 50 kilos d’ATP par jour.
Si le corps est à court de l’ATP, il peut en produire de très petites quantités directement à partir du glucose en le convertissant en acide lactique. C’est exactement ce que de nombreuses personnes atteintes du syndrome de fatigue chronique font. Ils passent alors d’un métabolisme aérobie à un métabolisme anaérobie.
L’accumulation d’acide lactique dans le sang, appelée acidose lactique est associée à des douleurs musculaires, des lourdeurs, douleurs et courbatures ce qui endommage le muscle et le tissu nerveux. Pour ces raisons, les personnes souffrant du syndrome de fatigue chronique ont des difficultés à augmenter leur forme physique.
Le coenzyme Q 10
Une déficience en coenzyme Q 10 a été observée dans de nombreuses études. Le coenzyme Q 10 est un des éléments de la chaîne respiratoire mitochondriale permettant la synthèse d’ATP, l’énergie universelle utilisée par notre corps. En cas de carence en coenzyme Q 10, non seulement moins d’énergie sera produite mais, le stress oxydant sera également accru participant au cercle vicieux de ce syndrome.
Ce manque en coenzyme Q10 peut également expliquer la dépression rencontrée dans le syndrome de fatigue chronique ainsi que l’augmentation de morbidité par maladies cardiovasculaires.
Déficiences hormonales associées
Le cortisol
Les patients souffrant du syndrome de fatigue chronique ont souvent des taux de cortisol effondrés et de faibles doses d’hydrocortisone peuvent améliorer cette fatigue chez les patients ayant des taux bas de cortisol (4, 5, 6, 7)
La mélatonine
La mélatonine régule les rythmes de veille et de sommeil, une désynchronisation de l’organisme c’est-à-dire un déplacement (en avance ou en retard) de la phase du rythme circadien conduisant à des signes cliniques faits de fatigue, troubles du sommeil, troubles de l’humeur.
Chez les patients atteints de Parkinson et souffrant du syndrome de fatigue chronique, la prise de mélatonine diminue l’anxiété, améliore le sommeil ainsi que leur qualité de vie (8).
Chez certains patients souffrant du syndrome de fatigue chronique, le cycle nychtéméral est perturbé, la sécrétion de la mélatonine se fait plus tardivement et leur sommeil n’est donc pas réparateur. Chez ces patients, un traitement par mélatonine améliore significativement la fatigue (9).
L’ocytocine
Son nom signifie accouchement rapide en grec. Elle joue un rôle important lors de l’accouchement mais aussi lors de l’allaitement en renforçant les liens, elle a également un rôle apaisant entre une mère et son enfant ou entre deux amoureux, l’ocytocine renforce les comportements positifs, elle présente encore bien d’autres propriétés, l’une d’entre elle étant la diminution du stress reconnu comme facteur potentiellement déclenchant du syndrome de fatigue chronique. L’ocytocine régule nos émotions et notre comportement social (10, 11, 12, 13, 14, 15)
La vasopressine
Le syndrome de fatigue chronique est associée à des altérations de la sécrétion de la vasopressine (hormone antidiurétique) et l’activité nerveux autonome cardiovasculaire, ce qui suggère un dérèglement central et explique certains symptômes : un étourdissement ou une faiblesse en position debout, la fatigue ainsi qu’un état vaseux, confus. (16, 17, 18, 19, 20).
Les hormones thyroïdiennes
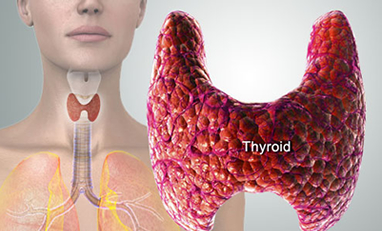 Les hormones thyroïdiennes sont indispensables au bon fonctionnement de nos cellules. Lorsque les hormones thyroïdiennes atteignent les cellules cibles, elles stimulent l’activité cellulaire qui libère de l’énergie thermique participant au maintien de notre température corporelle. En effet, l’hypothyroïdie peut s’accompagner de frilosité et de fatigue. Les signes cliniques d’hypothyroïdie peuvent être présents alors que les dosages sanguins se situent dans les normes du laboratoire. Tout comme pour la ménopause, il est donc important de se focaliser sur les signes cliniques. Si ceux-ci sont amendés par le traitement, il s’agit d’une hypothyroïdie subclinique.
Les hormones thyroïdiennes sont indispensables au bon fonctionnement de nos cellules. Lorsque les hormones thyroïdiennes atteignent les cellules cibles, elles stimulent l’activité cellulaire qui libère de l’énergie thermique participant au maintien de notre température corporelle. En effet, l’hypothyroïdie peut s’accompagner de frilosité et de fatigue. Les signes cliniques d’hypothyroïdie peuvent être présents alors que les dosages sanguins se situent dans les normes du laboratoire. Tout comme pour la ménopause, il est donc important de se focaliser sur les signes cliniques. Si ceux-ci sont amendés par le traitement, il s’agit d’une hypothyroïdie subclinique.
Parfois, la thyroxine (T4) pro-hormone ne peut se transformer en tri-iodothyroxine (T3) forme active. Cela se rencontre notamment en cas de stress facteur déclenchant du syndrome de fatigue chronique où la T4 se transforme en reverse T3 (rT3) forme inactive (21).
Si en prescrivant un mélange de T4 et T3 (Erfa Thyroïd), certains symptômes disparaissent tels que le manque d’énergie, la frilosité, la fatigue, ce test thérapeutique est concluant et cette substitution peut être poursuivie.
La DHEA
Le syndrome de fatigue chronique est associé à des taux bas de DHEA et la correction de ce déficit améliore cette fatigue chronique (22, 23)
La DHEA joue un rôle en régulant le système immunitaire et la réponse inflammatoire à l’origine de ce syndrome de fatigue chronique(24).
L’hormone de croissance
Le pic de sécrétion d’hormone de croissance survient entre 23 heures et 3 heures. L’hormone de croissance permet entre autre de récupérer de la fatigue physique et psychique accumulée au long de la journée.
La sécrétion nocturne en hormone de croissance a tendance à être réduite chez les patients souffrant du syndrome de fatigue chronique (25, 26).
Bien que la qualité de vie, ne se soit pas améliorée de manière significative au cours du traitement GH, certains patients ont pu reprendre le travail après une longue période de congé de maladie (27).
Le Bilan et la prise en charge
Vous serez invité à remplir un questionnaire santé.
Un bilan nutritionnel et hormonal exhaustif sera prescrit afin de cibler les causes de cette fatigue chronique et une prise en charge personnalisée vous sera proposée.
Guérir du syndrome de fatigue chronique
 En restituant une flore digestive “protectrice” et la fonction de barrière intestinale, l’inflammation peut être contrôlée et de nombreux symptômes tels que les troubles gastro-intestinaux, la fatigue, l’insomnie, les douleurs musculaires…disparaîtront.
En restituant une flore digestive “protectrice” et la fonction de barrière intestinale, l’inflammation peut être contrôlée et de nombreux symptômes tels que les troubles gastro-intestinaux, la fatigue, l’insomnie, les douleurs musculaires…disparaîtront.
La maîtrise de l’excès du stress oxydant accroîtra la production d’énergie. La correction des déséquilibres hormonaux est également l’une des clefs de la guérison.
Bibliographie
1. Association québécoise de la douleur chronique
2. Gut inflammation in chronic fatigue syndrome. Shaheen E Lakhancorresponding and Annette Kirchgessner. Nutr Metab (Lond)v.7; 2010PMC2964729.
3. Irritable bowel syndrome and other functional gastrointestinal disorders. Şimşek I. J Clin Gastroenterol. 2011 Aug; 45 Suppl:S86-8.
4. Hypothalamo-pituitary-adrenal axis dysfunction in chronic fatigue syndrome, and the effects of low-dose hydrocortisone therapyCleare AJ, Miell J, Heap E, Sookdeo S, Young L, Malhi GS, O’Keane V. . J Clin Endocrinol Metab. 2001 Aug; 86(8):3545-54.
5. Diurnal patterns of salivary cortisol and cortisone output in chronic fatigue syndrome. Jerjes WK, Cleare AJ, Wessely S, Wood PJ, Taylor NF. J Affect Disord. 2005 Aug; 87(2-3):299-304.
6. 24-hour pituitary and adrenal hormone profiles in chronic fatigue syndrome. Di Giorgio A, Hudson M, Jerjes W, Cleare AJ. Psychosom Med. 2005 May-Jun; 67(3):433-40.
7. The role of hypocortisolism in chronic fatigue syndrome. Nijhof SL, Rutten JM, Uiterwaal CS, Bleijenberg G, Kimpen JL, Putte EM. Psychoneuroendocrinology. 2014 Apr; 42:199-206. doi: 10.1016/j.psyneuen.2014.01.017. Epub 2014 Jan 30.
8. The use of melatonin in the treatment of chronic fatigue syndrome and circadian rhythm disorders in Parkinson’s disease. Datieva VK, Rosinskaia AV, Levin OS. Zh Nevrol Psikhiatr Im S S Korsakova. 2013; 113(7 Pt 2):77-81.
9. Influence of melatonin on fatigue severity in patients with chronic fatigue syndrome and late melatonin secretion. Van Heukelom RO1, Prins JB, Smits MG, Bleijenberg G. Eur J Neurol. 2006 Jan;13(1):55-60. http://www.ncbi.nlm.nih.gov/pubmed/16420393
10. Oxytocin enhances resting-state connectivity between amygdala and medial frontal cortex. Sripada CS, Phan KL, Labuschagne I, Welsh R, Nathan PJ, Wood AG. Int J Neuropsychopharmacol. 2013 Mar;16(2):255-60.
11. Modulation of Resting-State Amygdala-Frontal Functional Connectivity by Oxytocin in Generalized Social Anxiety Disorder. Dodhia S, Hosanagar A, Fitzgerald DA, Labuschagne I, Wood AG, Nathan PJ, Phan KL. Neuropsychopharmacology. 2014 Mar 5.
12. Early life stress modulates amygdala-prefrontal functional connectivity: Implications for oxytocin effects. Fan Y, Herrera-Melendez AL, Pestke K, Feeser M, Aust S, Otte C, Pruessner JC, Böker H, Bajbouj M, Grimm S. Hum Brain Mapp. 2014 May 26.
13. Oxytocin enhances resting-state connectivity between amygdala and medial frontal cortex. Sripada CS, Phan KL, Labuschagne I, Welsh R, Nathan PJ, Wood AG. Int J Neuropsychopharmacol. 2013 Mar; 16(2):255-60.
14. Intranasal oxytocin increases positive communication and reduces cortisol levels during couple conflict. Ditzen B, Schaer M, Gabriel B, Bodenmann G, Ehlert U, Heinrichs M. Biol Psychiatry. 2009 May 1; 65(9):728-31.
15. Sex-specific effects of intranasal oxytocin on autonomic nervous system and emotional responses to couple conflict. Ditzen B, Nater UM, Schaer M, La Marca R, Bodenmann G, Ehlert U, Heinrichs M. Soc Cogn Affect Neurosci. 2013 Dec;8(8):897-902.
16. Hormonal alterations in adolescent chronic fatigue syndrome. Wyller VB, Evang JA, Godang K, Solhjell KK, Bollerslev J. Acta Paediatr. 2010 May;99(5):770-3.
17. The neuroendocrinology of chronic fatigue syndrome and fibromyalgia. Psychol Med. 2001 Nov;31(8):1331-45. Parker AJ, Wessely S, Cleare AJ.
18. Abnormalities in response to vasopressin infusion in chronic fatigue syndrome. Altemus M, Dale JK, Michelson D, Demitrack MA, Gold PW, Straus SE. Psychoneuroendocrinology. 2001 Feb; 26(2):175-88.
19. Desmopressin augments pituitary-adrenal responsivity to corticotropin-releasing hormone in subjects with chronic fatigue syndrome and in healthy volunteers. Scott LV, Medbak S, Dinan TG. Biol Psychiatry. 1999 Jun 1; 45(11):1447-54.
20. Chronic fatigue disorders: an inappropriate response to arginine vasopressin? Peroutka SJ. Med Hypotheses. 1998 Jun; 50(6):521-3.
21. Supraphysiological cyclic dosing of sustained release T3 in order to reset low basal body temperature. Friedman M, Miranda-Massari JR, Gonzalez MJ. P R Health Sci J. 2006 Mar;25(1):23-9.
22. http://www.nlm.nih.gov/medlineplus/druginfo/natural/331.html
23. Symptoms, signs and laboratory findings in patients with chronic fatigue syndrome. Kuratsune H, Yamaguti K, Hattori H, Tazawa H, Takahashi M, Yamanishi K, Kitani T. Nihon Rinsho. 1992 Nov;50(11):2665-72.
24. Decreased dehydroepiandrosterone sulfate but normal insulin-like growth factor in chronic fatigue syndrome (CFS): relevance for the inflammatory response in CFS. Maes M, Mihaylova I, De Ruyter M. Neuro Endocrinol Lett. 2005 Oct;26(5):487-92.
25. Secretion of growth hormone in patients with chronic fatigue syndrome. Berwaerts J, Moorkens G, Abs R. Growth Horm IGF Res. 1998 Apr;8 Suppl B:127-9.
26. Changes in growth hormone, insulin, insulinlike growth factors (IGFs), and IGF-binding protein-1 in chronic fatigue syndrome. Allain TJ, Bearn JA, Coskeran P, Jones J, Checkley A, Butler J, Wessely S, Miell JP. Biol Psychiatry. 1997 Mar 1;41(5):567-73.
27. Effect of growth hormone treatment in patients with chronic fatigue syndrome: a preliminary study. Moorkens G1, Wynants H, Abs R. Growth Horm IGF Res. 1998 Apr;8 Suppl B:131-3.
28. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Maes M1, Leunis JC. Neuro Endocrinol Lett. 2008 Dec;29(6):902-10.




